Weighing High Deductible Medical Insurance: Who Benefits?
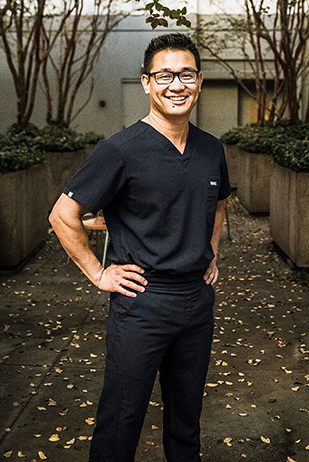
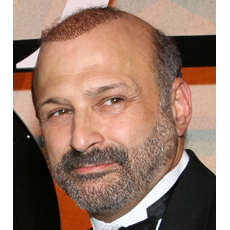
Wayne Lipton, Managing Partner, Concierge Choice Physicians
Americans have an unquenchable thirst for the best–and that means healthcare too. But does more care translate necessarily to better care? How much is too much? Is some care not necessary? And most importantly, who decides?
If you are one of many Americans who now have a high-deductible insurance plan, you are the one deciding. In a high deductible plan, patients pay for their initial care, up until a certain point, when insurance kicks in. These plans are less expensive than traditional insurance plans because the cost of care is shifted to patients. The idea is that if patients have to pay for care themselves, utilization will be better controlled. But does this save the system money in the long run? And is it fair?
Based on my perspective, I would say the answer to both questions is a resounding “no.” Sadly, utilization control by patients has devolved into denial of care, particularly for lower income patients. This is a far cry from years ago, when indemnity insurance plans did not include co-pays or deductibles. Patients and employers paid their insurance premium, and visits were covered. Physicians were happy to offer as much service as patients demanded, since they were paid for the volume of work they provided.
Because there was no incentive for either the patient or the physician to reduce the number of services to what was truly necessary, and every reason to maximize the number of services, utilization became unmanageable and needlessly expensive. To control utilization, a co-pay was introduced, forcing patients to put a little skin in the game. By having to pay for some portion of the visit, patients had to consider whether they really needed to visit their doctor.
Sounds reasonable. But the co-pay concept obviously put a higher burden on lower income people. In fact, during the last economic recession, visit rates to physicians decreased ― not because people were less sick, but rather, they could not afford the co-pays. Now, for many people, it’s not just the expense of a co-pay ― deductibles have grown into thousands of dollars annually. What is the impact on the patient, and in the long run, the cost of care?
High deductible plans can cause pervasive and insidious problems for our health care system, depending where you fit on the economic strata. For individuals and employee groups, they have a much greater negative impact on those with lower salaries. They also discriminate against older people, sicker people and those with chronic conditions. Beyond the obvious economics ― much more so than with co-pays ― patients who may need treatment decide they cannot pay the cost, and choose not to take care of issues, or delay treatment until things become serious. In this regard, high deductible plans begin to look much more like the major medical insurance plans that existed 50 years ago, where catastrophic care was covered, versus primary care as a universal benefit.
In concept, utilization control is supposed to help manage the unnecessary care that costs all of us money. But if people are delaying care until the point of no return, smaller issues like an infection that could be handled by a primary care physician with a simple antibiotic can ultimately result in an exponentially more expensive treatment in a hospital with a specialist. How is this saving money? A high deductible plan is inconsistent with an individual’s need for healthcare by construct.
In the end, there is a cost to care, and it has to come from somewhere. Accentuating the dialog are critical questions that need answers now: Is healthcare a right that should be covered for everyone? Should patients not be obligated to pay for it directly, or should they be personally responsible for it? What is the most effective role for insurance? Should it cover everything, or only the most expensive costs like a hospitalization, surgery or high-cost treatments?
And, for the sake of countless Americans delaying care due to the financial burdens, how can we manage utilization more effectively to cover the necessary items while avoiding those that fall in a gray area?
Wayne Lipton has more than 35 years of experience in healthcare and business, including the past 11 years as founder and managing partner of Concierge Choice Physicians, LLC. He has conducted hundreds of seminars on full-model and hybrid concierge practices.